Policies
A payer policy spells out what is covered, what is not covered, and other details of the agreement between the patient and the payer.
Use the Payers > Policies tab to identify the policy type. You can associate multiple policy types to a single insurance but you cannot identify two of the same type such as two commercial policies. Each benefit plan must be associated with a policy, so it is important to identify all the payer’s policies first before configuring the benefit plans.
Add a policy
-
Click Payers on the navigation bar.
-
On the Payers page, find and click the payer name.
-
Click the Policies tab.
-
Click Add a policy.
-
Enter the required information and then click Save.
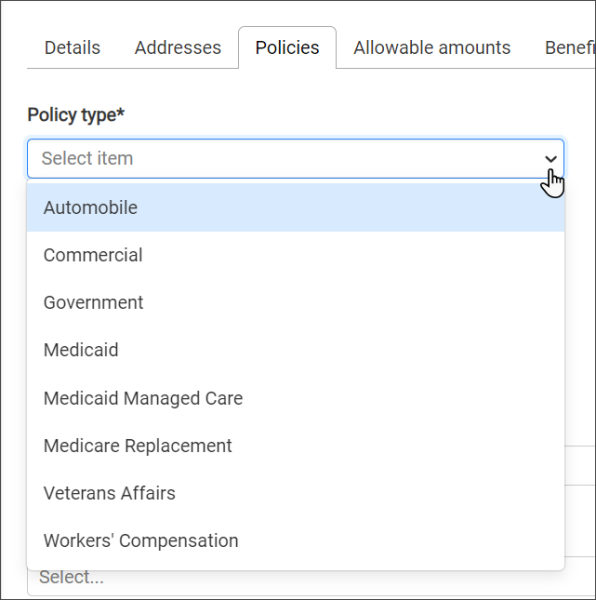
Policy type: Select the policy type from the drop-down menu.
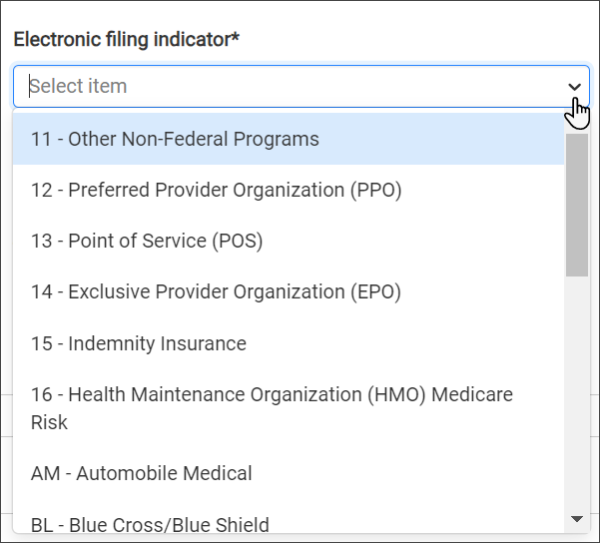
Electronic filing indicator: An electronic filing indicator is used on ANSI 837 and ANSI 837P (Professional) standard format used to electronically transmit health care claims.
Clearinghouse fields: These fields are optional.
Provider ID: Enter your National Provider Identifier (NPI) here. Your NPI is a 10-digit number required by HIPPA for all healthcare providers in the United States. It is used to identify your company in all HIPPA transactions. If you don’t know your NPI, look it up here: https://npiregistry.cms.hhs.gov. If you don’t have an NPI, call 1800-465-3202.
Provider ID override: If you need to override the provider ID, ZOLL provides two options, 24J RenNPI - Tax ID and 24J RenProvNum -Blank.
Carrier code: Some Medicaid providers need carrier codes for secondary electronic submissions. The carrier codes are published by payer. These codes are not set or maintained by ZOLL Billing.
Primary submission: Select the submission type to use when this payer is the primary payer.
Secondary submission: Select the submission type to use when this payer is the secondary payer.
Timely filing claims: Amount of time the insurance company allows for claim submission. If the timely filing is 90 days, you have up to 90 days from the claim's date of service to submit the claim.
Timely filing appeals: The amount of time the insurance company allows for a claim appeal.
Requirements: We have a whole section that explains each requirement and what they do. Check out Payer requirement settings.
Primary authorization requirements: Used to require a claim authorization number when that specific LOS is selected for this payer.
Sequestration: A mandatory 2% payment reduction in the Medicare FFS Program. Select an option from this field to regulate how the system applies sequestration.
Mileage rounding: You have several options when reporting mileage. You can round the number up, down, or not at all (fractional). Click this field and select the option that describes how you report mileage.
Note: If the primary payer on a submitted or completed claim is changed and the new payer uses a different mileage rounding type, the original mileage charge is obsoleted, and the new payer's mileage rounding setting is applied to the claim.
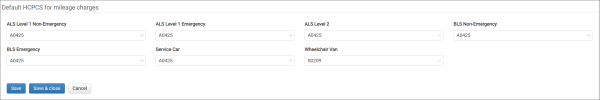
Medicaid set default HCPCS for mileage charges
Set the mileage HCPCS for Medicaid.
Note: This setting only persists if this Medicaid payer is the primary payer.
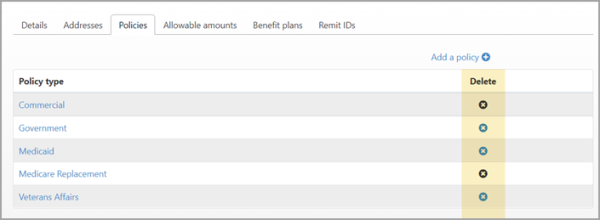
Delete a policy
A policy can be deleted if it is not associated with a claim. The X will be disabled if the policy cannot be deleted.
If the X is enabled (blue), on the same line as the policy you wish to delete, click the X under the Delete column.