Release 13.9.2 (10.17.2024)
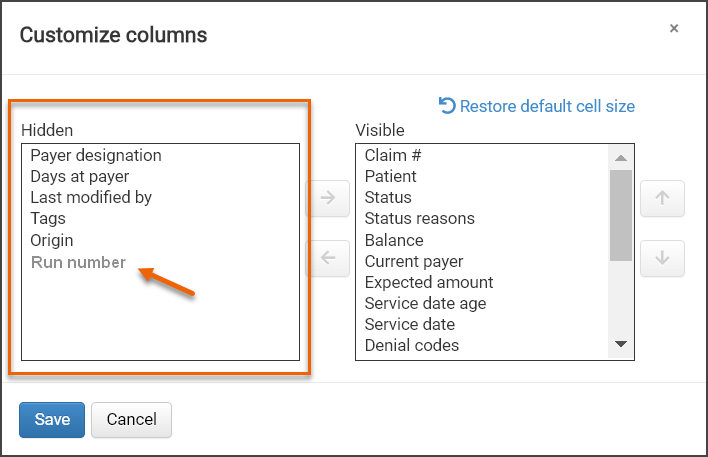
Run number added to column options for Inbox
The Inbox displays a series of informational columns that can be customized to suit your preferences. In this release, we’re giving you the option to add a new column that shows the run number. By default, it will be hidden, but when visible, it will function like other existing columns.
Mass adjustments via Advanced Search Results page
Important! This feature functionality has been delayed until 10/31.
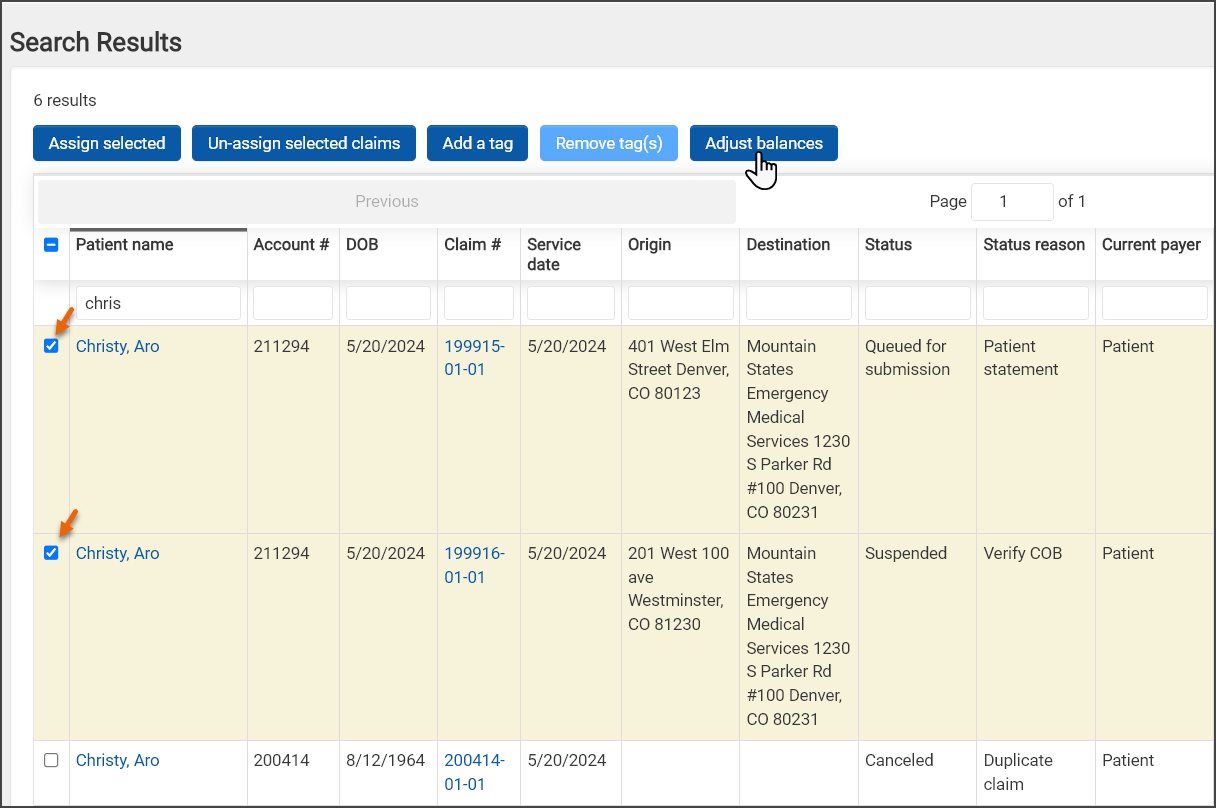
Using the Advanced Search Results page, you can now adjust the balance of multiple claims at one time (1,000 claim limit).
-
On the top navigation bar, click "Advanced."
-
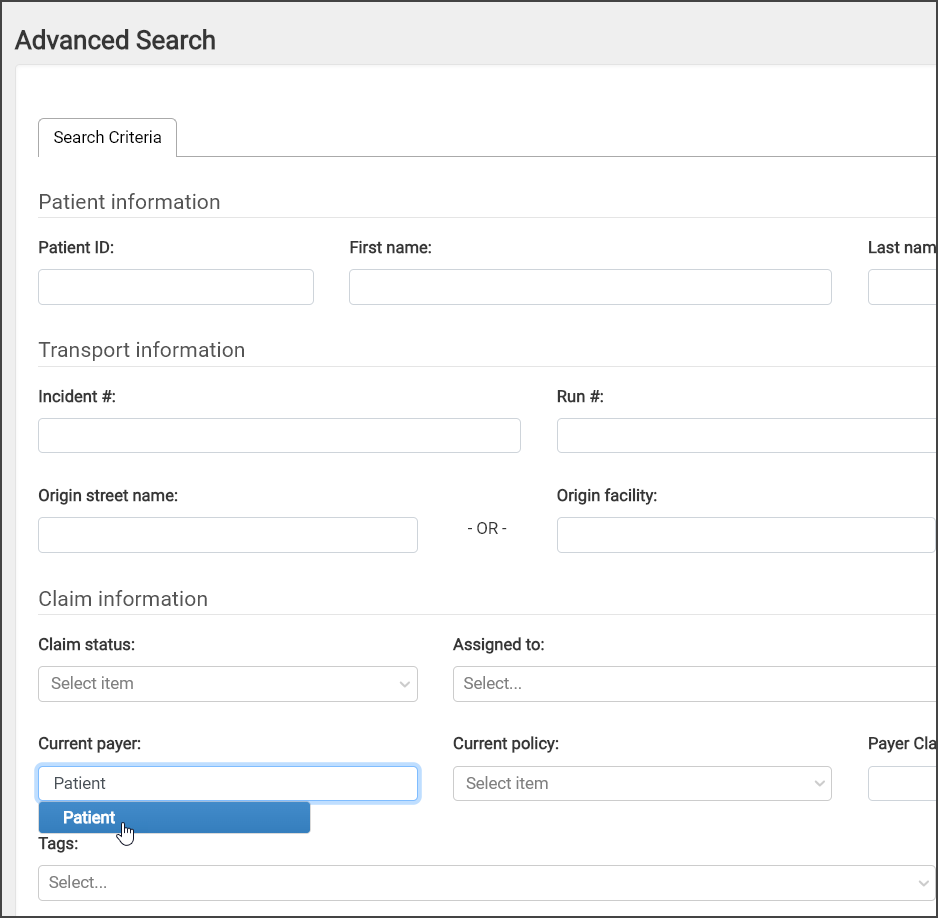
On the Advanced Search page, enter the criteria that will allow the claims to display on the results page.
-
On the Advanced Search Results page, use the check boxes on the left of each line to select the claims you want to adjust.
-
After the selection is complete, click the "Adjust balances" button at the top of the page.
-
On the Adjust balances window:
-
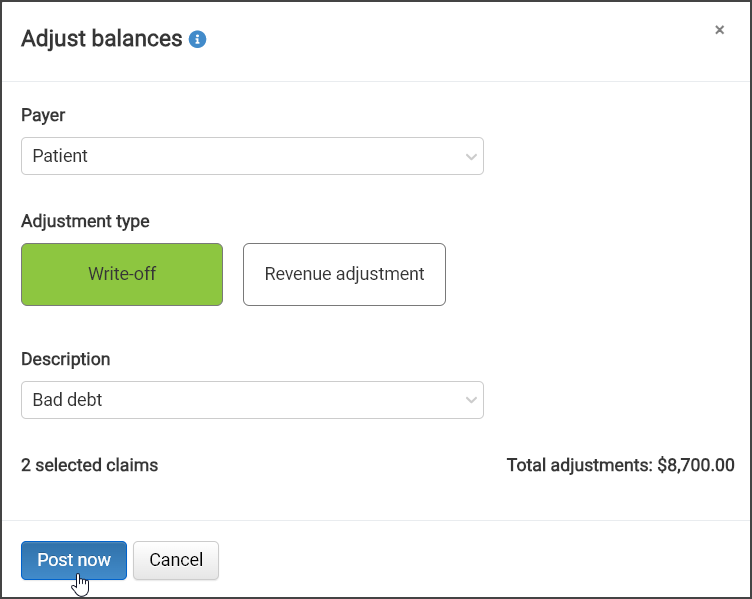
Payer: Click the Payer field and then select the payer from the list. A couple of things to note about this list:
-
This field defaults to patient.
-
If specific payers were used for the advanced search, the list will be limited to those payers.
-
Only those payers that are active on the claim's COB will display.
-
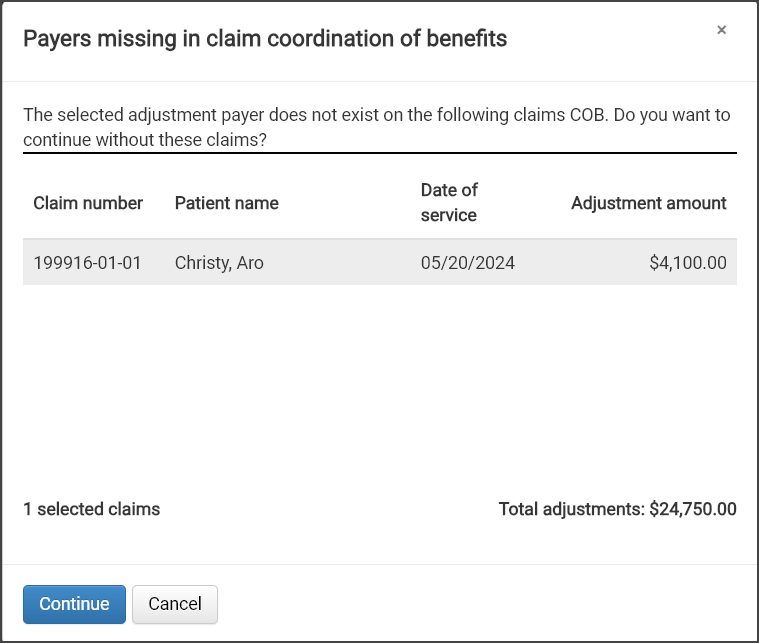
The payer must be on the COB of all the selected claims and have a payer claim record. If that is not the case, a window will display that shows the claim(s) in question and explains that the payer is missing in the claim's COB. You can continue the adjustments without the listed claim(s).
-
-
Adjustment type: Select either write-off or revenue adjustment.
-
Description: Click the field and then select a description from the list.
Note the number of affected claims and the sum of the total adjustment amount that displays under the Description field.
-
Click the "Post now" button.
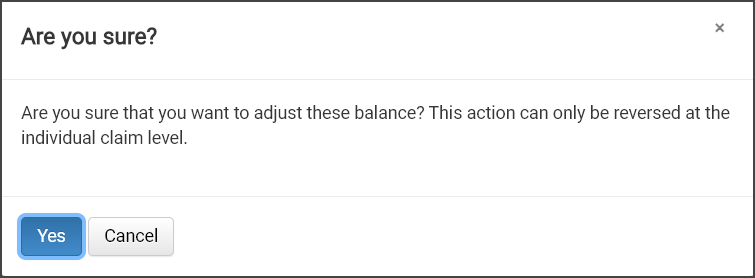
If this action needs to be reversed, you will need to do it on the individual claim level. To ensure that you understand this point, a confirmation message will display and you will be required to acknowledge that message by clicking Yes to complete the transaction.
-
Color enhancement
You may notice that some of the buttons and links look a little different in this release. That is because we update the blue color on all the Billing pages to obtain a more cohesive look and feel.
Improved performance
Multi-company Management (MCM) customers with many defined charges were sometimes experiencing an inability to complete a claim and long load times on the Claim page > Charges tab. This issue was addressed in 13.9.2 resulting in the ability to complete the claim regardless of the number of defined charges and shorter load times when viewing charges.
Insights update
Insights now supports more than three years of data.
The following issues were fixed in release 13.9.2:
-
Patient Responsibility tab was incorrectly showing that a single patient claim was submitted to Waystar multiple times.
-
There were cases where the profit center was not being populated on the claim when it was created because the latitude and longitude data was not included in the NEMSIS file. To address this, a new hierarchy of checks will now be used to determine the appropriate profit center for the claim:
-
Lat/long
-
Origin address or cross streets
-
Zip code - Note that since a zip code can fall under multiple profit centers, this method may lead to inaccuracies. In such cases, the Biller should verify the correct profit center.
-
-
A $0.00 amount was received for a claim's line item that included a claim level adjustment (such as PI238) for the full claim balance. When a user posted the $0.00 to the claim and the next payer was the patient, the system was not sending out patient statements.
-
When users moved and then removed a claim to collections or state debt, the claim was not going out for automatic submission to the clearinghouse.
-
Deductible Monitoring: Claims with -1 days remaining in the Deductible Monitoring queue were not being automatically submitted. For the incomplete claim > Hold for Deductible message, we now use DOS for calculating the maximum days release date instead of today's date.
-
The ZOLL Dispatch record was not attaching to PCRs for one customer.
-
Patient statements did not include payments received from an inactive payer.