Posting a Single Payment
-
Click Payments on the navigation bar and then click Payments.
-
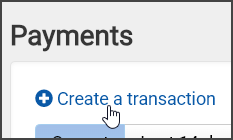
On the Payments page, click "Create a transaction."
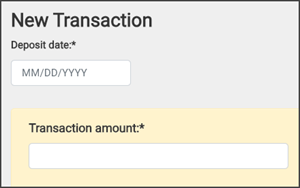
On the New Transaction page, the fields on the top are mandatory.
-
Click in the "Deposit date" field and enter the deposit date.
Click in the "Transaction amount" field and enter the transaction amount.
-
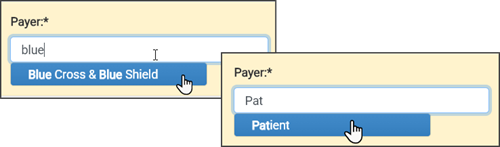
Click in the "Payer" field and start typing the payer name and then select it from the list. If this is a patient payer, start typing "patient" in this field and then select patient.
-
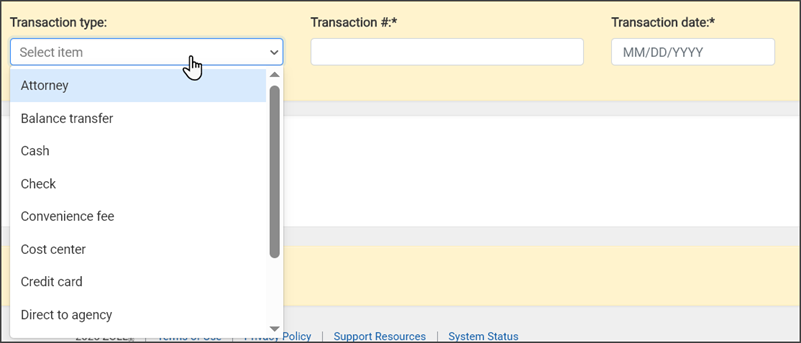
Click in the "Transaction type" field and enter type of payment.
-
Click in the "Transaction #" field and enter the transaction number. If this is a check, enter the check number here.
-
Click in the "Transaction date" field and enter the EOB date or if this is a check, enter the date the check was issued.
-
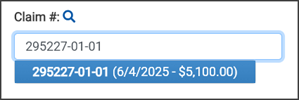
If you have the claim number, click in the "Claim #" field and enter or paste the claim number. If you do not have the claim number, click the search icon and find the claim by first or last name and service date.
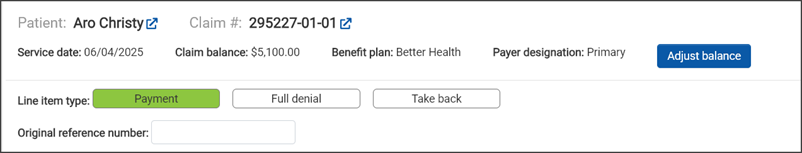
The charge information displays.
There are several things you can do on this page. You can adjust the balance, add a claim note, identify the line item type such as payment, full denial or takeback, and enter a reference number.
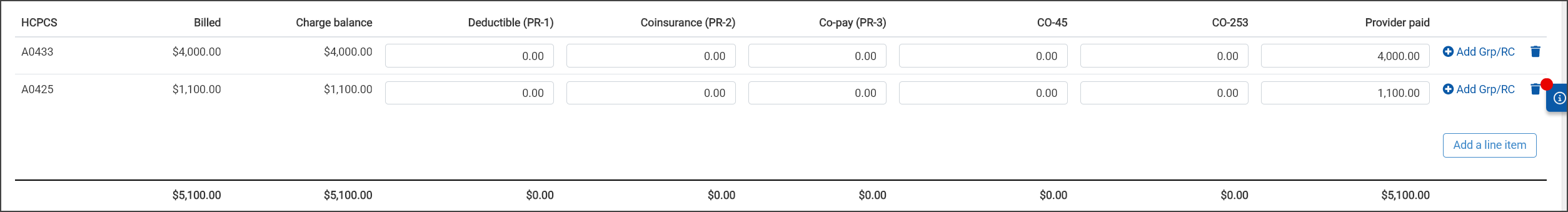
The amount owed displays per HCPCS. You can adjust the amount in any field. Just remember that the provider paid amount must match the transaction amount before you can post this payment.
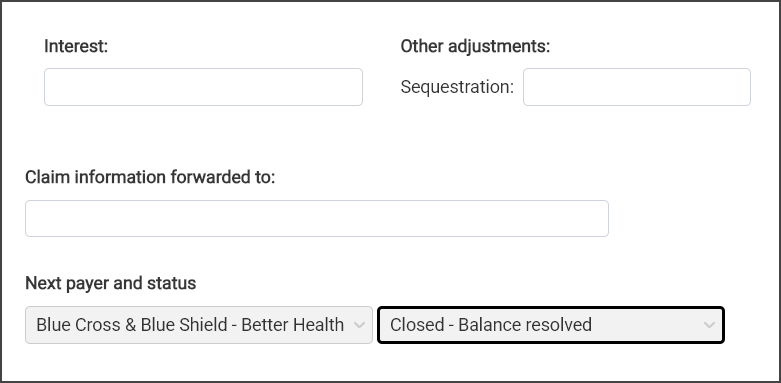
If the payment is made in full, the "Next payer and status" at the bottom of the page will show "Closed – Balance resolved." If this is a partial payment, you can adjust the next payer and the status if needed.
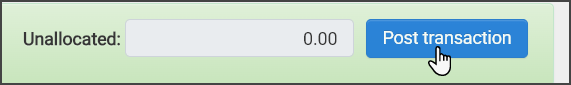
If the information is correct, scroll to the bottom of the page. If the unallocated field equals zero, the bar will be green and you're ready to post. If the bar is green and the "Post transaction" button is not enabled, ensure that the mandatory fields are filled out. If the bar is yellow, there is an issue that you must address before you can post.
Note: The Provider Paid amount must equal the Transaction amount to turn the bar green and enable the "Post transaction" button.
A confirmation message tells us that the transaction was successfully applied to the claims.