Coverage Status (Eligibility)
- Matching your payer name with payer in Eligibility service
- What to do if you get a not eligible response
- Running coverage status from the Claim page
Run Coverage Status when you think you know the patient's insurance but need to verify it, or you are sure the patient has insurance but you are missing information.
The coverage status link displays in the insurance description on the Coordination of Benefits tab. This tab displays on the Claim Creation pages and on the Claim page. Eligibility can be run for any payer at any time regardless of designation.
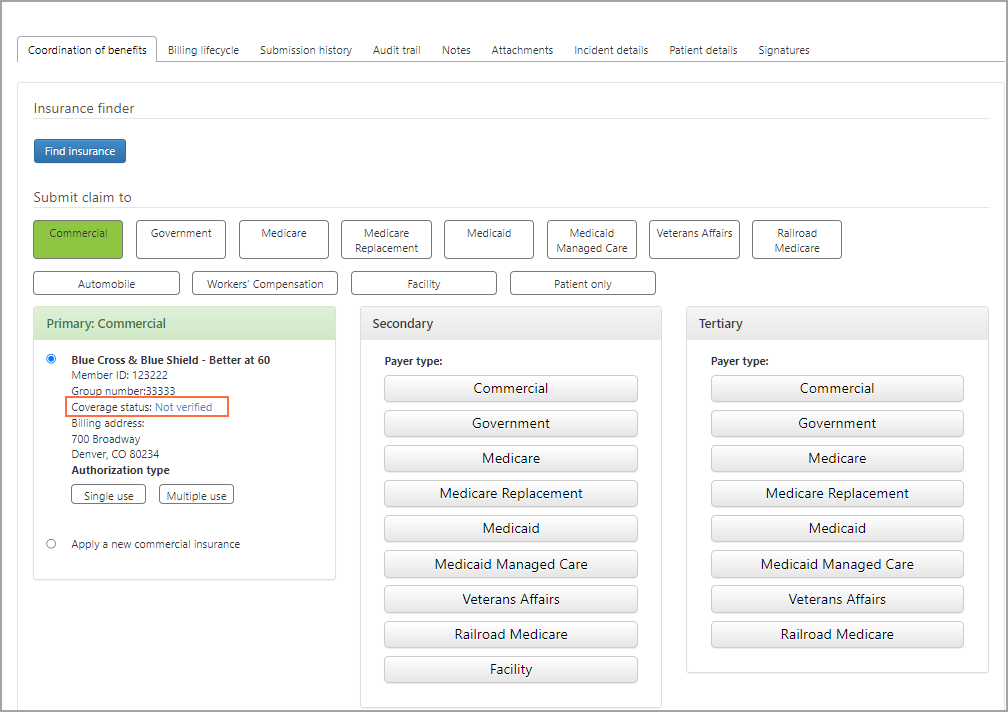
The link name next to "Coverage status" indicates the status of the eligibility check:
- Not verified: This payer has not yet been verified - click to run eligibility.
- Inactive: The insurance is no longer active for this patient - change the payer to Patient and run Insurance Discovery ('find insurance for this patient').
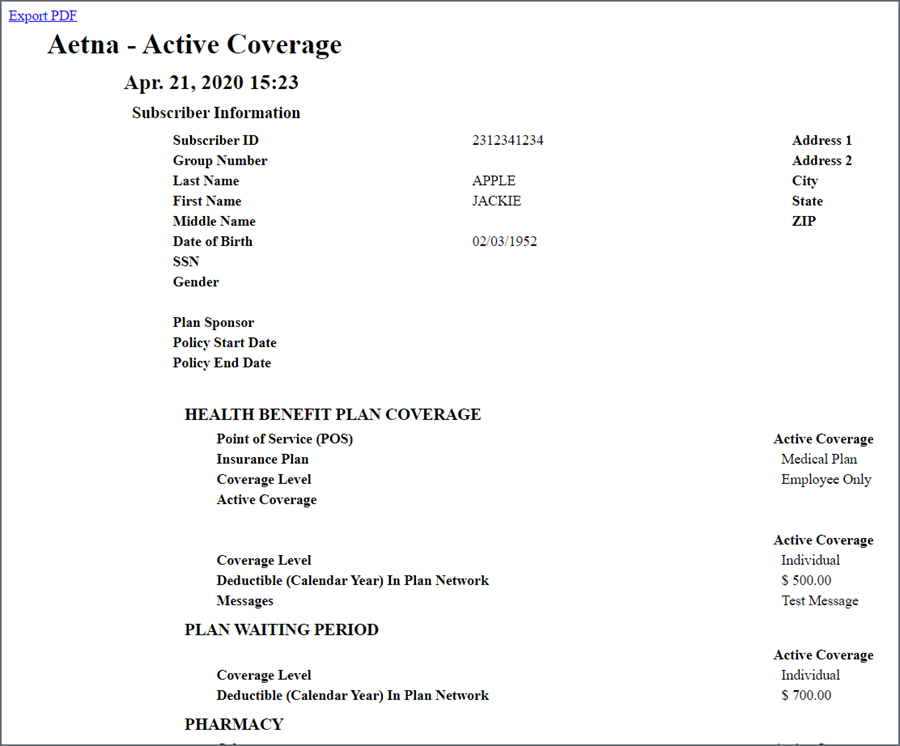
- Eligible: Patient has insurance - click to view Active Coverage sheet.
- Not found: No insurance was found - bill the patient.
Matching your payer name with payer in Eligibility service
Because you have the ability to name payers anything you want, your payer name may not match the payer's legal name in the ZOLL Eligibility service. To correct this problem, when you run eligibility on a payer for the first time, you will be presented with the following window.
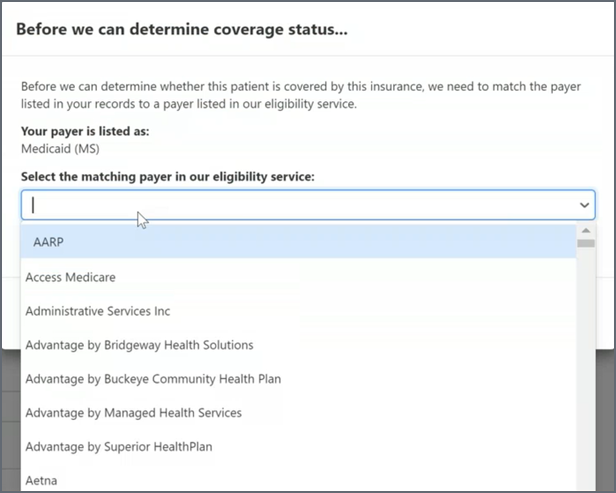
Click the field and select the payer in the list that matches the payer in your system.
Now, click Continue. Your payer is now matched with the payer you selected. You only have to do this once! The system will remember the matching from this point forward.
What to do if you get a not eligible response
If the response is anything other than "Eligible", the system places the claim in a suspended status. For example, if the response is 'Inactive', the claim status changes to "Suspended - Inactive coverage", or if the response is "Not found", the claim status changes to "Suspended - Verify coverage." The change in the claim's status is an indication that the coordination of benefits requires your attention. If the claim status changes to suspended, run Insurance Discovery and see if the patient has additional or different coverage that you can use.
Running coverage status from the Claim page
You can run coverage status anytime from the Claim page > "Coordination of benefits" tab.
- Go to the Claim page. You can do this by entering the claim number in Search then clicking the claim number link on the search response page.
- On the Claim page, click the Coordination of benefits tab (this tab opens by default).
- For every payer, under the "Coverage status" column you will either see a status with an icon next to it or "Not verified."
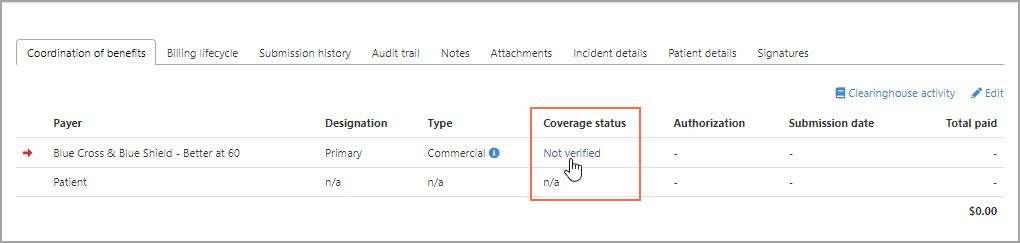
- If the coverage status is anything besides "Not verified", click the icon next to the status to open the "Coverage status history" window.
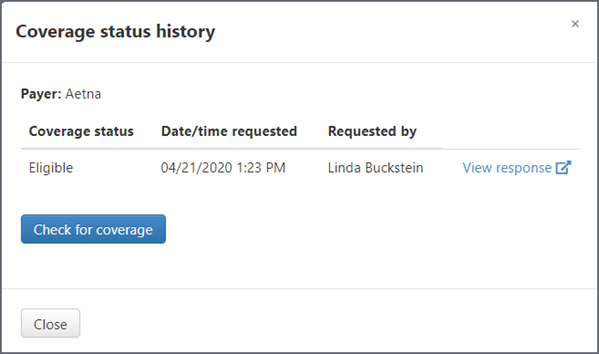
Click View response to see response details in a different tab. If needed, you can export this response to a PDF.