Add Payer After Patient Invoice
After submitting the invoice for services to the patient, you may find that the patient had insurance that was not on your records. Use these steps to add a payer to the claim after the invoice was submitted to the patient:
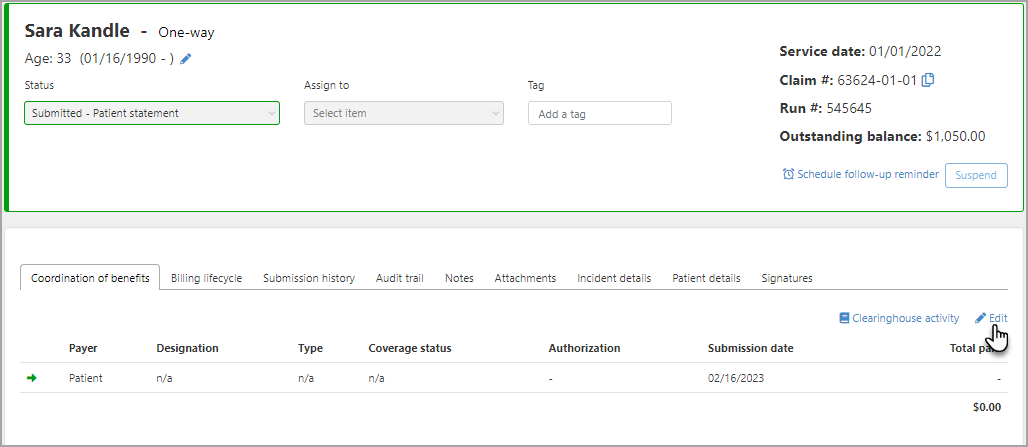
- Enter the claim number in the search field. On the results window, click the claim number to view the claim. The claim's status will be Submitted - Patient statement.
- On the Coordination of benefits tab, click Edit.
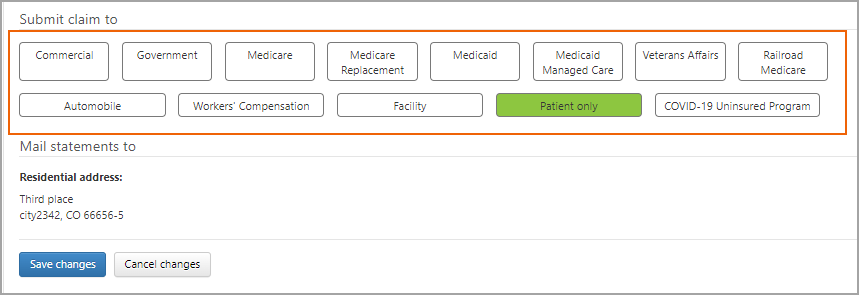
- Select the button that represents the payer type for primary.
- In the primary box, enter the payer information and then click Save changes.
- Click Queue for submission.